Every year, 1.5 million Americans admitted to the intensive care unit (ICU) experience a serious adverse drug event (or ADE). Additionally, it is estimated that every one of the 5 million critically ill patients will experience at least one medication error during their ICU stay. Even more alarming than these numbers is that the risk of mortality doubles for each severe ADE, and the associated healthcare costs to treat these ADEs exceeds $1 billion.
One College of Pharmacy faculty member believes that healthcare can be made safer and more affordable through using artificial intelligence-based information technology to provide real-time ADE prediction that can guide clinicians at the bedside to prevent errors. The Agency for Healthcare Research and Quality (AHRQ), who serves as the leading Federal agency for improving safety and quality of healthcare in the United States, has backed her theory with $2.15 million dollars in funding in the form of two grants awarded in 2022.

Dr. Andrea Sikora
Dr. Andrea Sikora, a Clinical Associate Professor at the College of Pharmacy and critical care pharmacist at AU Medical Center, has been awarded a $1.86 million R01 Grant from AHRQ. Her winning application, “Artificial intelligence-based health IT tools to optimize critical care pharmacist resources through adverse drug event prediction,” was officially awarded August 29th. The award complements a $296,000 R21 grant that Dr. Sikora received earlier this year from AHRQ entitled, “Machine learning validation of medication regimen complexity for critical care pharmacist resource prediction.”
Dr. Sikora’s vision is to “provide data-driven, optimal pharmacotherapeutic care for every critically ill patient.” A key step to providing optimal pharmacotherapeutic care is ADE prevention, a formidable challenge. Yet, with the proper tools and timely intervention, these ADEs are preventable, especially through the care of specially trained ICU pharmacists.
“ICU patients suffer three times more adverse drug events and higher medication errors than any other patients because of their complex, high-risk drug regimens, but we have a solution for this: critical care pharmacists! Research indicates that critical care pharmacists integrated into the healthcare team reduce ADEs by 70% because they make preventative medication interventions. But a key problem to implementing this solution is that the critical care pharmacist workload is not optimized. We need technology solutions that support pharmacists.”
The challenge, Sikora explained, is twofold: First, not all ICU patients receive the care of a critical care pharmacist. Second, if they do have a pharmacist, those critical care pharmacists are often responsible for an excessively high number of ICU patients, making it more difficult to catch those errors. High ICU workloads for ICU healthcare workers are associated with increased mortality risk.
“To make patient care safer, more efficient, and more equitably distributed, information technology strategies that optimize critical care pharmacy resources are needed. Our plan is to develop a clinician-friendly health IT tool that will visualize artificial intelligence informed predictions from the perspective of the critical care pharmacist who will ultimately prevent those adverse drug events,” said Sikora.
To date, large volumes of complex, dynamic data generated by critically ill patients has posed a significant barrier to predicting ADEs at the bedside. The field has lacked robust prediction models that use validated metrics to guide critical care pharmacists in safe medication use. “Using artificial intelligence to predict adverse drug events is an exciting solution to improve quality and effectiveness of healthcare delivery,” she added. “Artificial intelligence offers powerful analytical techniques capable of handling Big Data like that generated in the ICU. Those techniques have never been tested in the setting of improving medication safety through critical care pharmacist-driven interventions and that is what we are setting out to do.”
In particular, her team will evaluate a novel, data-driven health IT metric she developed in 2016 called the Medication Regimen Complexity-Intensive Care Unit (MRC-ICU) Scoring Tool. Dr. Sikora likes to quote Robert Sharma, “’What gets measured, gets improved.’ This is the point of the MRC-ICU- measurement to improve practice.”
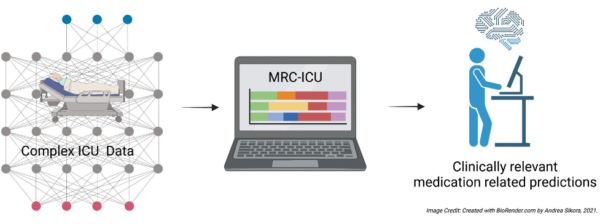
Complex ICU patient data will be harnessed using artificial intelligence techniques with the novel MRC-ICU Scoring Tool to provide clinically relevant medication predictions for clinicians at the bedside to reduce ADEs.
She explained, “Evaluating the MRC-ICU Scoring Tool will be our first step in building an artificial intelligence-based prediction model. Our compelling preliminary data suggest that MRC-ICU is a valid metric for intervention, and our hypothesis is that an artificial intelligence-informed dashboard visualizing medication outcomes causal pathways will provide critical care pharmacists with an actionable tool to improve patient-centered outcomes.”
Progress on the work of Dr. Sikora and The MRC-ICU Investigator Team can be followed here.
Dr. Sikora noted that “this work is not possible without the support and mentorship from the outstanding MRC-ICU Investigator Team.” This team includes critical care pharmacists, intensivists, biostatisticians, computer scientists specializing in machine learning, and human factors engineers. In particular, long-time MRC-ICU collaborator and fellow College of Pharmacy colleague and UGAC3 member Dr. Susan Smith, is one of Dr. Sikora’s co-investigators on this project. Three other University of Georgia faculty are also key collaborators including Drs. Shen (College of Public Health), Li (College of Computer Science), and Liu (College of Computer Science). Additional co-investigators include Drs. Devlin, Murphy, Kamaleswaran, Kandaswamy, Murray, Buckley, and Rowe. She noted that there is a fascinating overlap between the interconnected neural networks of machine learning algorithms and the mentorship and collaboration networks that support team science. “In neural networks you can ‘feed forward’ and in mentorship you can ‘pay it forward’,” she observed. This inspiration has led her to publish a book on the topic of mentorship in healthcare: Pay It Forward: A Map to Mentorship in Medicine.